In a recent study, obesity was divided into two unique subcategories, each of which has its own effects on how our bodies work. The discovery may not only help us diagnose weight-related health disorders more precisely, but it may also help us treat them in more individualized ways.
Body mass index (BMI) measures are currently used to diagnose obesity, but the team behind the new research claims that this method is overly simplistic and runs the danger of being deceptive by disregarding individual biological variances.
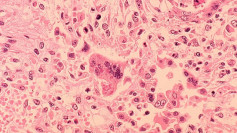
One of the recently discovered kinds of obesity is characterized by a higher fat mass, whereas the other has both a higher fat and lean mass. Unexpectedly, the researchers discovered the second type was accompanied by elevated inflammation, which has been connected to a higher risk of cancer and other illnesses.
"Using a purely data-driven approach, we see for the first time that there are at least two different metabolic subtypes of obesity, each with their own physiological and molecular features that influence health," J. Andrew Pospisilik, an epigenetics researcher studying metabolic disease at the Van Andel Institute in Michigan said. "Translating these findings into a clinically usable test could help doctors provide more precise care for patients."
The researchers identified four metabolic subtypes that affect body mass, two of which are predisposed to leanness and two of which are predisposed to obesity, using information from 153 pairs of twins gathered as part of the TwinsUK research project.
Using mice that were genetically identical, were raised in the same environment, and consumed the same amount of food, these findings were subsequently confirmed in laboratory mouse models.
The validity of these findings was subsequently confirmed in laboratory mouse models using mice that were genetically identical, were raised in the same setting, and consumed the same amount of food.
These controls imply that something additional than diet, environment, and genetics is occurring. Epigenetic markers, which are non-coding changes made to DNA molecules and alter how genes are read, are one possible cause. Twins with the same DNA code aren't always identical, which is explained by epigenetics.
As far as the researchers can tell, the chance appears to be the primary cause of the second sort of obesity, the one connected to inflammation. As a result, these findings may also be relevant to the study of unexplained phenotypic variation (UPV), which is the hypothesis that influences other than our genes and environment shape who we are.
In order to develop standards that doctors may use to diagnose them differently, researchers are now looking to further examine the two types of obesity they've identified.