The World Health Organization (WHO) has declared the ongoing mpox outbreak in Africa a global health emergency, marking a critical juncture in the fight against a virus that has rapidly spread across the continent. The declaration, announced on Wednesday, comes as a more virulent strain of mpox, known as clade Ib, has been detected in four new provinces in Africa, raising alarm among health experts and government officials alike.
The decision to elevate the mpox outbreak to the status of a Public Health Emergency of International Concern (PHEIC) follows an urgent meeting of independent experts who advised WHO Director-General Tedros Adhanom Ghebreyesus on the severity of the situation. "This is something that should concern us all," said Tedros. "The potential for further spread within Africa and beyond is very worrying."
The PHEIC designation is the highest level of alert under international health law, reserved for extraordinary events that pose a public health risk through the international spread of disease. This status typically necessitates a coordinated global response to prevent further escalation, and in this case, WHO is calling for immediate international cooperation to contain the outbreak.
The African continent has been hit hard by mpox, a viral disease formerly known as monkeypox, which has spread to 13 countries and resulted in over 17,000 reported cases and more than 500 deaths since the beginning of the year. The Democratic Republic of Congo (DRC) is at the epicenter of the outbreak, accounting for over 96% of all confirmed cases. "We are now in a situation where mpox poses a risk to many more neighbors in and around central Africa," warned Salim Abdool Karim, chair of the Africa CDC emergency group.
The outbreak has been particularly devastating among children, with nearly 70% of cases in the DRC involving individuals under 15 years old. Tragically, children also account for 85% of the deaths. The spread of the virus in refugee camps in eastern Congo has been especially concerning, where overcrowding and poor sanitary conditions have exacerbated the crisis. Jacques Alonda, an epidemiologist working in the region, recounted the harrowing case of a six-week-old baby who contracted mpox just two weeks after birth due to the conditions in an overcrowded hospital.
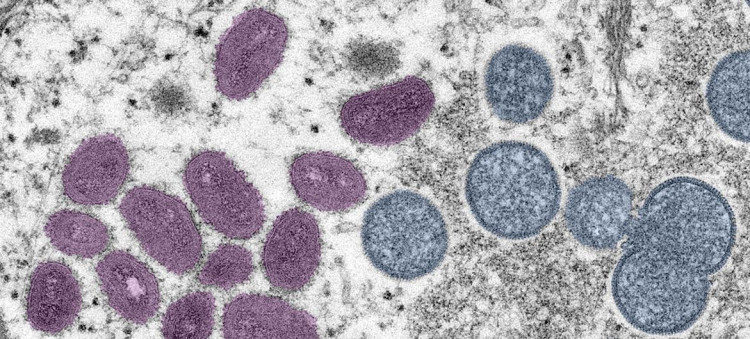
The rapid spread of clade Ib, a more transmissible and deadly form of mpox, has heightened concerns among health officials. This strain, which has a mortality rate of approximately 3-4%, was previously contained to the DRC but has now reached Burundi, Kenya, Rwanda, and Uganda. The emergence of this strain underscores the urgent need for a robust international response to prevent further devastation.
WHO has already initiated the Emergency Use Listing process for mpox vaccines and is working on a regional response plan that requires $15 million in funding. To date, $1.45 million has been released from the WHO Contingency Fund for Emergencies. However, the availability of vaccines and treatments in Africa remains limited, exacerbating the challenges faced by health authorities on the ground.
The global response to previous mpox outbreaks has been inconsistent, with Western countries largely containing the virus in 2022 through the use of vaccines and treatments. However, the African continent has not benefited from the same level of support. "It's a failure of the global community that things had to get this bad to release the resources needed," said Michael Marks, a professor of medicine at the London School of Hygiene and Tropical Medicine.
In the absence of sufficient mpox vaccines, some experts have suggested using smallpox vaccines, which are related to mpox, to inoculate populations at risk. However, the logistics of deploying such a strategy remain complex, particularly in regions where healthcare infrastructure is already strained by other epidemics such as measles, cholera, and malnutrition.
Despite the WHO's emergency declaration, there are concerns that it may not be enough to galvanize the global community into action. Dr. Boghuma Titanji, an infectious diseases expert at Emory University, emphasized that the previous emergency declaration for mpox in 2022 "did very little to move the needle" on delivering critical resources like diagnostic tests, medicines, and vaccines to Africa. "The world has a real opportunity here to act in a decisive manner and not repeat past mistakes," she warned, but added that achieving this will require more than just an emergency declaration.