We have heard several of our patients recovering from COVID-19 tell us these even months after their initial diagnosis as pulmonologists and critical care physicians caring for patients with lung disease. They may have survived the most dangerous part of their sickness, but they haven't yet recovered to their pre-COVID-19 baseline, finding it difficult to accomplish things like heavy lifting and laundry.
One in five American people with COVID-19 has had these long-lasting consequences, also known as extended COVID. Numerous symptoms, including brain fog, fatigue, coughing, and shortness of breath, are associated with long COVID.
The Biden-Harris administration places a special emphasis on research to better understand the causes of protracted COVID because these symptoms can be brought on by harm to or dysfunction of numerous organ systems.
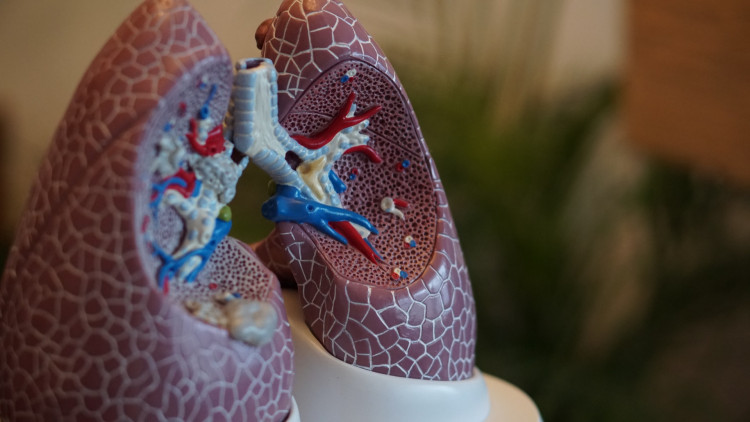
Although the lungs are not always involved in breathing issues, they are frequent. What may lie ahead for certain patients following a COVID-19 infection can be better understood by taking a closer look at the basic functioning of the lungs and how they can be impacted by the disease.
The lungs' primary job is to supply the body with oxygen-rich air and eliminate carbon dioxide. The blood is brought into close contact with the air as it enters the lungs, allowing oxygen to diffuse into the body and carbon dioxide to diffuse out. Even though it seems straightforward, this process necessitates amazing synchronization between blood flow, also known as perfusion, and airflow, or ventilation.
A type of lung disease is when the body's airways are blocked. Asthma and chronic obstructive pulmonary disease are two prominent causes of impairments like these. In some patients who have recovered from COVID-19, researchers have noticed persistent airway blockage.
Restriction, or trouble expanding the lungs, is a different type of lung illness. The amount of air that the lungs can hold is reduced by restriction, which also reduces the size of the lungs. The development of scar tissue, also known as fibrosis, in the lungs as a result of damage frequently leads to restriction. Researchers have also discovered that COVID-19 survivors, particularly those who had a severe illness, are susceptible to developing restrictive lung disease in the future.
Last but not least, if blood flow to the alveoli, where gas exchange takes place, is compromised, the lungs cannot perform their role even if airflow and lung capacity are unaffected. Blood clot risk is elevated with the presence of COVID-19. A potentially fatal pulmonary embolism that reduces blood flow to the lungs can be brought on by blood clots that make their way to the lungs. However, there is proof that severe COVID-19 infections can directly harm lung blood vessels and reduce blood flow while the patient is recovering.
In these three common ways, the function of the lungs can be compromised, and COVID-19 can cause all of them. The best approaches to cure the persistent lung damage brought on by lengthy COVID are still being worked out by scientists and medical professionals.