GLP-1 medications, originally developed to treat type 2 diabetes, are increasingly being used for weight loss, according to a recent study by Cedars-Sinai Medical Center. This trend is causing concerns about potential drug shortages and limited access for diabetic patients who need these medications.
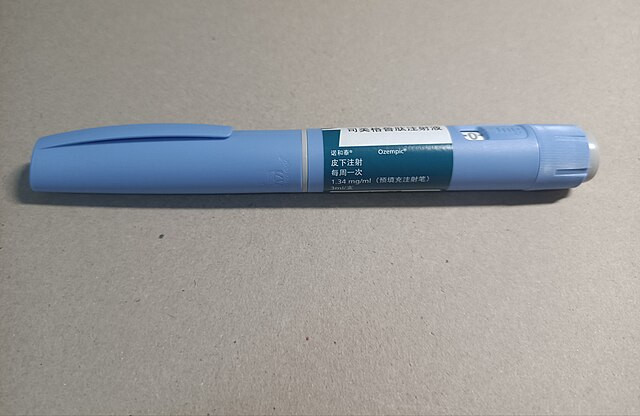
The study, published in the Annals of Internal Medicine, analyzed approximately 1 million first-time GLP-1 prescriptions in the U.S. from 2011 to 2023. Researchers found that while the number of new patients prescribed GLP-1 drugs for diabetes decreased by nearly 10% during this period, prescriptions for obesity and related health conditions more than doubled, particularly since 2020. Notably, Novo Nordisk's semaglutide-marketed under brand names such as Ozempic, Wegovy, and Rybelsus-accounted for over 88% of all new GLP-1 prescriptions in 2023.
Dr. Yee Hui Yeo, co-first author of the study and a clinical fellow in the Karsh Division of Gastroenterology and Hepatology at Cedars-Sinai, emphasized the implications of this trend. "The growing popularity of GLP-1 medications among those with obesity could exacerbate a nationwide drug shortage," Yeo stated. "This raises concerns about the need to ensure that patients with diabetes still have access to these treatments."
GLP-1 drugs work by lowering blood sugar levels and interacting with the brain to suppress appetite, making patients feel full longer. They have been approved by the FDA for both diabetes and weight management, with semaglutide and liraglutide being the most commonly prescribed for weight loss. Despite their effectiveness, the surge in demand has led to shortages, affecting both the U.S. and Europe. The European Medicines Agency has warned that the shortage is a "major public health concern" that may persist into 2024.
The study's findings align with a broader trend in the weight loss industry, which analysts estimate could be worth $100 billion by 2030. This growing market is driven by increasing awareness and acceptance of medical treatments for obesity. However, the surge in off-label use of GLP-1 drugs by individuals who do not meet the FDA's criteria for obesity or related health conditions has also contributed to the shortages. Dr. Nancy Rahnama, an internal and bariatric medicine specialist in Beverly Hills, described this off-label use as "abuse," warning that these individuals are "far more likely to develop serious side effects."
Common side effects of GLP-1 drugs include gastrointestinal issues such as nausea, vomiting, and diarrhea. These side effects, along with the high cost of the drugs, have led to a significant discontinuation rate among diabetic patients. According to a study by Northwestern Medicine, almost 40% of patients on second-line diabetes drugs, including GLP-1s, stop treatment, with the rate rising to 50% among GLP-1 users.
Dr. Ali Rezaie, medical director of the Cedars-Sinai GI Motility Program and co-first author of the study, noted the dramatic rise in GLP-1 prescriptions for obesity. "After the medication was approved for obesity, GLP-1 drug use took off so quickly that we lost control and vision of how fast people were picking up these medications," Rezaie said. The study also revealed that most new GLP-1 users are white women with a body mass index (BMI) of 30 or higher, considered obese.
In response to the shortages, the FDA's database indicates that several GLP-1 medications, including certain doses of Wegovy, Mounjaro, Zepbound, Saxenda, and Victoza, remain in short supply. The shortages have prompted some diabetics to ration their medications, as reported by NPR.